Rustenhoven J, Drieu A, Mamuladze T, de Lima KA, Dykstra T, Wall M, Papadopoulos Z, Kanamori M, Salvador AF, Baker W, Lemieux M, Da Mesquita S, Cugurra A, Fitzpatrick J, Sviben S, Kossina R, Bayguinov P, Townsend RR, Zhang Q, Erdmann-Gilmore P, Smirnov I, Beatriz-Lopes M, Herz J, Kipnis J. Cell. Feb 18, 2021; 184(4):1000-1016.e27.
Abstract
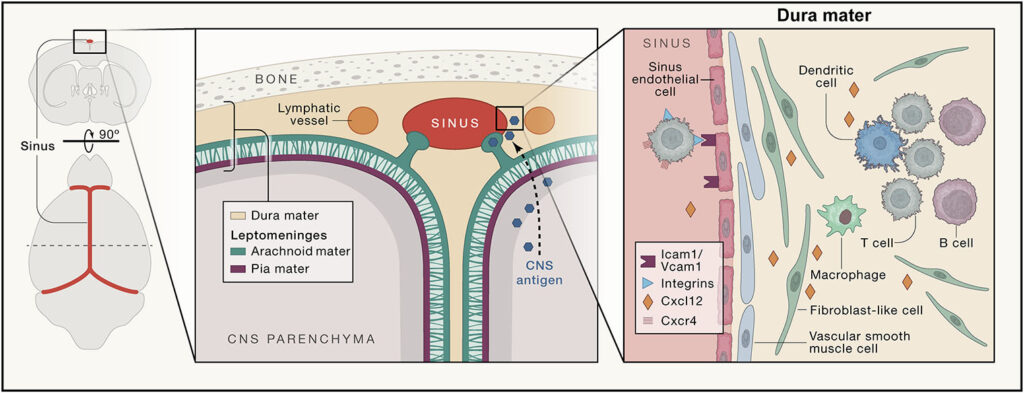
Despite the established dogma of central nervous system (CNS) immune privilege, neuroimmune interactions play an active role in diverse neurological disorders. However, the precise mechanisms underlying CNS immune surveillance remain elusive; particularly, the anatomical sites where peripheral adaptive immunity can sample CNS-derived antigens and the cellular and molecular mediators orchestrating this surveillance. Here, we demonstrate that CNS-derived antigens in the cerebrospinal fluid (CSF) accumulate around the dural sinuses, are captured by local antigen-presenting cells, and are presented to patrolling T cells. This surveillance is enabled by endothelial and mural cells forming the sinus stromal niche. T cell recognition of CSF-derived antigens at this site promoted tissue resident phenotypes and effect or functions within the dural meninges. These findings highlight the critical role of dural sinuses as a neuroimmune interface, where brain antigens are surveyed under steady-state conditions, and shed light on age-related dysfunction and neuroinflammatory attack in animal models of multiple sclerosis.
Department mini interview
In this article, you describe a mechanism by which patrolling immune cells, from the peripheral immune system, survey cues about the immune status of the brain that accumulate in the cerebrospinal fluid surrounding the brain. You show that this is orchestrated by a number of players that make the meningeal sinuses an interface specialized in gathering and presenting brain-derived antigens to the immune system. What makes these findings so unique and impactful?
Justin Rustenhoven: I think a lot of the uniqueness and impact comes from the diverse pathologies this system could be involved in. For instance, we speculate that it could represent a site of antigen sampling in multiple sclerosis, considering that we see endogenous myelin proteins in the dura mater both in mouse models of the disease and humans affected by the disease. This could be involved in the initiation of the autoimmune attack. Many other pathologies, including neurodegenerative diseases like Alzheimer’s and Parkinson’s disease, also display circulating T cells recognizing brain antigens. It thus appears increasingly likely that T cells’ reactivation through recognition of their cognate antigen could be detrimental as a result of a massive inflammatory response. In other conditions like brain tumors, or even CNS infections, the pathway we describe could give the peripheral immune system a glimpse of what is going on in the brain. Importantly, this would occur without entrance of immune cells in the brain proper. Such ability to survey the CNS and respond to perturbations in the absence of barrier breakdown, which occurs in most pathologies, makes this quite a unique immune mechanism.
Textbooks teach our students about the so-called immune privilege of the central nervous system. Here, you found that the immune system does keep tabs on the brain, but from a distance, like a creepy neighbor that would go through your trash. So, does your study contradict or fuel the old dogma?
Jony Kipnis: It does not contradict the fact that the brain is immunologically unique, but it challenges the underlying mechanisms that have been previously proposed. The immune system sees brain-derived antigens, yet the responses towards protein coming from the brain are not as aggressive as they are in the periphery. What contributes to these unique immune responses? This is still a big question, and we are working in the lab to address it.
What spurred this study? How did it start?
Jony Kipnis: We have been fascinated with neuro-immune interactions for years now and the question was how the two systems communicate and where? Once we found meningeal lymphatics in the meninges, it became clear that brain borders have been overlooked for years and we decided to look closer. And then the “white elephant” stood right there in the middle of the room – it was impossible not to see it. Once you are up to something robust and obvious, all the experiments just fall into place.
This is such a comprehensive study, how many years of work and revisions went in to this publication?
Justin Rustenhoven: It’s hard to say exactly when a study starts but I’ve been with Jony for about three years now and the entire time has been centered around immune trafficking in and out of the central nervous system. We first submitted about 2 years after joining the lab, and got generally favorable, but extensive reviews. These really helped to shape the paper and over a 6-month period we ended up adding about twice as much data as was in the first version, but all of it proved valuable. Revisions were interesting, to say the least, as we got them right in the middle of an entire lab move from the University of Virginia (literally in the car drive down) and a global pandemic so we were working in shifts. Thankfully, many of the members of the Kipnis lab stepped in and helped, and having such fantastic people at the core facilities (WUCCI, GTAC@MGI, Flow Cytometry & Fluorescence Activated Cell Sorting Core, and the Proteomics Core Laboratory) proved absolutely essential to answering some of the tricky reviewer comments.
What new therapeutic avenues do you think your work is the most likely to open? Are you working on any?
Jony Kipnis: The immediate ones are autoimmune diseases of the brain (we are focusing on animal models of multiple sclerosis), brain tumors (on which we collaborate with Gavin Dunn’s lab now), meningeal and brain infections and likely many others. Ten years ago, most neuroscientists would have laughed at me (they actually laughed at me!) had I told them that the immune system may be playing a role in neurological disease. Today, I doubt there are any neurological diseases where the immune system is not playing some role. If that is the case, meningeal spaces may be a therapeutic target for many neurological diseases. It is an easily accessible area too – so does not have all the hurdles for drug delivery as the brain parenchyma does.